Study of Autoregulation Monitoring in Babies (SAMBA study)
Our research group is interested in developing new approaches to monitoring and imaging the neonatal brain, principally using optical techniques.
Figure 1 Neonate monitored by brain monitoring software
The SAMBA study is a project designed to understand the control of cerebral blood flow (CBF) to the brain of preterm infants (figure 1). There are a number of near-infrared spectrophotometers (NIRS) each providing a quantitative measurement of tissue oxygen saturation. Our group uses the Hamamatsu NIRO 200NX, which displays alongside changes in oxyhaemoglobin (HbO2) and deoxyhaemoglobin (HHb), the Tissue Oxygenation Index (TOI) and Tissue Haemoglobin Index (THI), a measure of oxygenation and blood volume, respectively.
Changes in brain oxygenation in premature babies essentially reflect changes in CBF to the brain. By comparing changes in the baby’s arterial blood pressure (ABP) with change in CBF we can get information on how well the cerebral circulation is being regulated – a process known as cerebral autoregulation. In healthy babies, CBF remains relatively constant over a wide ABP range, however in sick infants this control is lost and any fluctuations in ABP is probably transmitted to the brain. This leaves the brain vulnerable to low (ischaemia) and high CBF causing intraparenchymal haemorrhage.
Wong et al. were the first to investigate the relationship between TOI and mean ABP using coherence and transfer function analysis (TFA). High coherence was observed in sick preterm infants, indicating impaired cerebral autoregulation, and it was strongly associated with mortality.[1] Subsequently, using the same methodology, high coherence between TOI and mean ABP was observed at relatively low ABP variability in the sickest infants. This may indicate that the autoregulatory plateau is very narrow in these infants.[2]
Gilmore et al. used time domain analysis, described the cerebral oxygenation index (COx) – a moving and linear correlation coefficient between slow waves of mean ABP and NIRS derived loco-regional cerebral oxygen saturation (rSO2 ) – to study the autoregulation. They observed that lower ABP during the first 3 days of life was significantly associated with an impaired autoregulation in preterm infants <30 weeks gestation.[3]
Our group has described a novel index of cerebral vascular reactivity using the correlation coefficient between slow waves of TOI and the heart rate (HR) – known as the tissue oxygenation-heart rate reactivity index, TOHRx. Impaired vascular reactivity (positive values of TOHRx) was associated with higher CRIB II scores (figure 2). Using TOHRx we have been able to define values of MABPopt where cerebrovascular reactivity is strongest (figure 3). Preterm infants who died or had worse germinal matrix-intraventricular haemorrhages had a higher mean absolute deviation from MABPopt than patients who survived.[4-6]
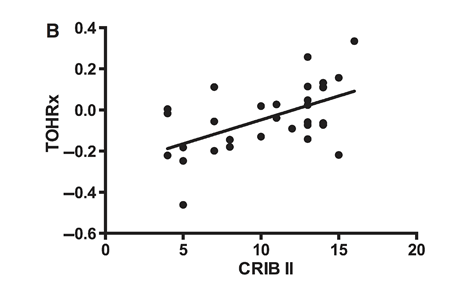
Figure 2 Regression analysis between tissue oxygenation-heart rate reactivity index (TOHRx) and the clinical risk index for baby’s (CRIB II) (p < 0.0015, R = 0.55) [4]
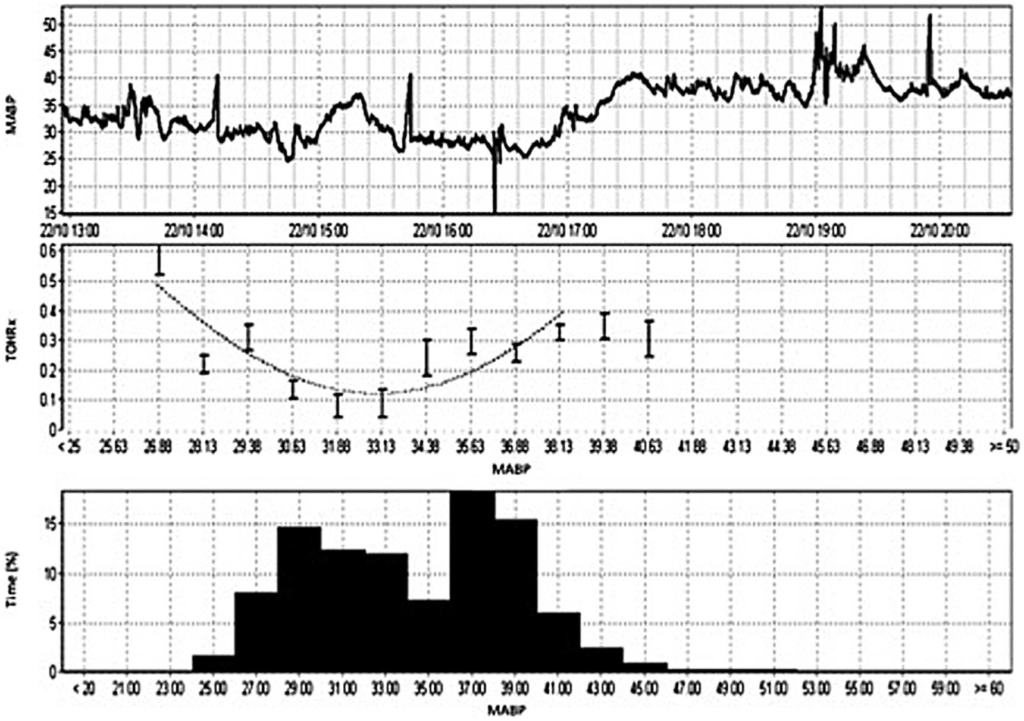
Figure 3 Example of TOHRx over mean arterial blood pressure (MABP) plot to determine the MABPopt in a single neonate: a male preterm infant born at 25+2 weeks’ gestational age with a birth weight of 860 g who was studied within his first 36 hrs of life for 23 hrs. This infant was ventilated and was not on inotropes during the recording study period. The first graph shows the infant’s actual MABP during the recording period. The second graph shows the MABPopt curve. MABPopt is defined by the lowest values of TOHRx, in this case 0.1, corresponding to a MABP of 31–33 mmHg. The frequency histogram shows the percentage of time spent in each value of MABP. [4]
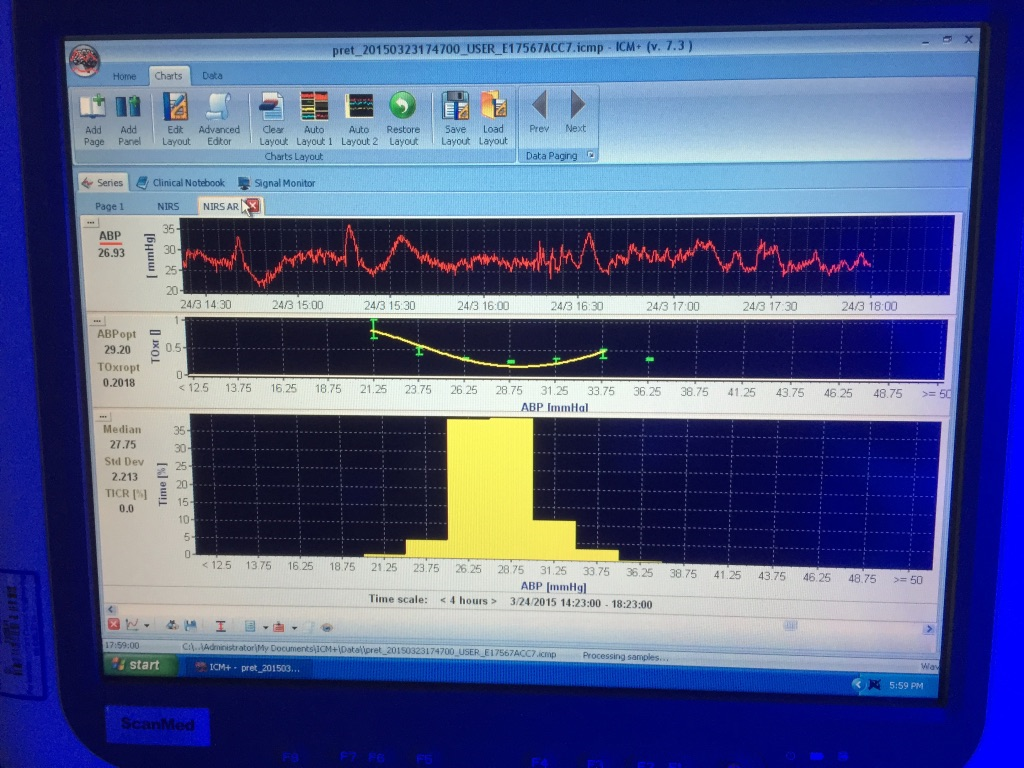
Figure 4 Cotside monitoring screen showing the time trend line for the arterial blood pressure (ABP) and the ABP-TOHRx error bar with fitted (U shape) curve with the corresponding ‘optimal’ ABP value (MABPopt = 29 mmHg). The ABP histogram showing the percentage of time that a certain value was present during 4 hour monitoring period.
For more information about the SAMBA study, please visit the website: www.neolabresearch.com
For further information:
Prof. Topun Austin: ta338@cam.ac.uk, Addenbrooke’s Hospital, Cambridge, United Kingdom.
Dr. Cristine Sortica da Costa: csortica@gmail.com, Addenbrooke’s Hospital, Cambridge, United Kingdom.
References
[1] Wong FY, Leung TS, Austin T, Wilkinson M, Meek JH, Wyatt JS, Walker AM. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy.Pediatrics. 2008 Mar;121(3):e604-11.
[2] Wong FY, Silas R, Hew S, Samarasinghe T, Walker AM.Cerebral oxygenation is highly sensitive to blood pressure variability in sick preterm infants. PLoS One. 2012;7(8):e43165.
[3] Gilmore MM, Stone BS, Shepard JA, Czosnyka M, Easley RB, Brady KM.Relationship between cerebrovascular dysautoregulation and arterial blood pressure in the premature infant. J Perinatol. 2011 Nov;31(11):722-9. doi: 10.1038/jp.2011.17. Epub 2011 Mar 3.
[4] Mitra S, Czosnyka M, Smielewski P, et al. T. Heart rate passivity of cerebral tissue oxygenation as an indicator of cerebrovascular reactivity in preterm infants. Acta Paediatr. 2014;103(9):e374-82.
[5] Costa CS, Czosnyka M, Mitra S, et al. Monitoring of cerebrovascular reactivity allows determination of optimal blood pressure in preterm infants. J Pediatr. 2015;167:86-91.
[6] Costa CS, Placed MM, Czosnyka M, et al. Complexity of brain signals is associated with outcome in preterm infants. JCBFM Jan 2017. 1:271678X16687314. doi: 10.1177/0271678X16687314.
