Monitored Brain Pathology
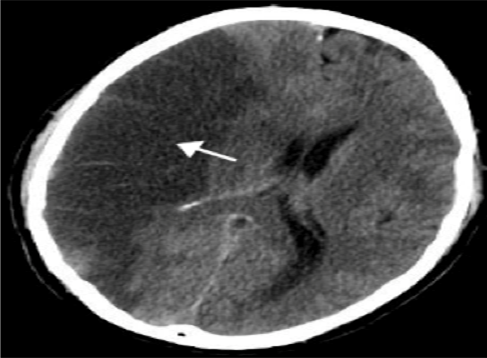
Traumatic Brain Injury: Traumatic brain injury is the most common cause of death and disability in young people, with an annual financial burden of over $50 billion per year in the United States. Traumatic brain injury is defined by both the initial primary injury and the subsequent secondary injuries (figure 1). Fundamental to emergency department management is ensuring brain perfusion, oxygenation, and preventing even brief or transient episodes of hypotension, hypoxia, and hypocapnia. Cerebral perfusion pressure is a function of intracranial pressure and systemic blood pressure, and it must be monitored and maintained. Current research is devoted towards the prevention and treatment of secondary injury. The emergency clinician must be vigilant in maintaining homeostasis while coordinating the downstream care of the patient, including the intensive care unit and/or the operating room.
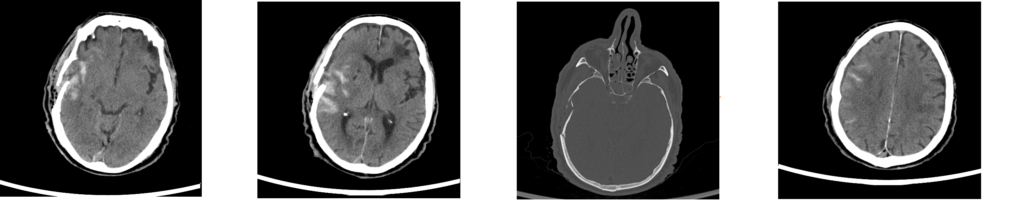
Subarachnoidal Haemorrhage: Subarachnoid haemorrhage (SAH) is a life-threatening type of stroke caused by bleeding into the space surrounding the brain (figure 2). SAH can be caused by a ruptured aneurysm, arteriovenous malformation (AVM), or head injury. One-third of patients will survive with good recovery; one-third will survive with a disability; and one-third will die. Treatment focuses on stopping the bleeding, restoring normal blood flow, and preventing vasospasm.
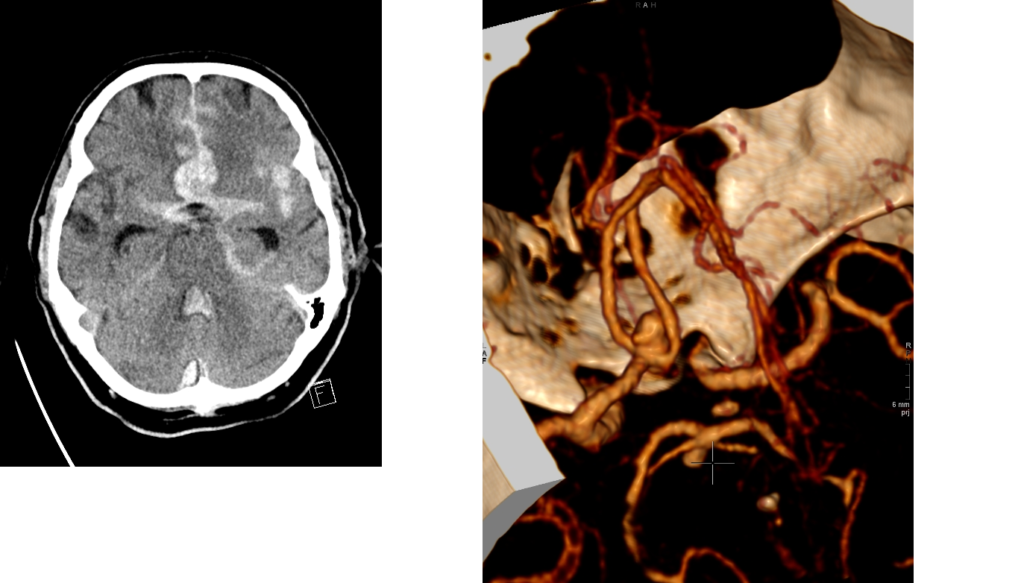
Spontaneous Intraparenchymal haemorrhage: Spontaneous haemorrhage into the cerebral parenchyma accounts for 8% to 13% of all strokes (figure 3). It is more common in males, in blacks, and in the elderly. Fifty percent of cases are due to the effects of chronic hypertension on intracranial perforating arteries. The basal ganglia are the most frequent site of bleeding. Lobar hematomas tend to occur in younger patients, and may be due to specific causes such as vascular malformations. Many patients will have increased intracranial pressure and will require treatment in an intensive care unit. Prognosis is related to the patient’s age and neurologic condition, and to the size, location, and rapidity of formation of the hematoma.

Ischemic stroke: Ischemic stroke occurs when an artery to the brain is blocked. The brain depends on its arteries to bring fresh blood from the heart and lungs. The blood carries oxygen and nutrients to the brain, and takes away carbon dioxide and cellular waste. If an artery is blocked, the brain cells (neurons) cannot make enough energy and will eventually stop working. If the artery remains blocked for more than a few minutes, the brain cells may die. This is why immediate medical treatment is critical. Ischemic stroke can be caused by several different kinds of diseases. The most common problem is narrowing of the arteries in the neck or head. This is most often caused by atherosclerosis, or gradual cholesterol deposition. If the arteries become too narrow, blood cells may collect and form blood clots. These blood clots can block the artery where they are formed (thrombosis), or can dislodge and become trapped in arteries closer to the brain (embolism). Another cause of stroke is blood clots in the heart, which can occur as a result of irregular heartbeat (for example, atrial fibrillation), heart attack, or abnormalities of the heart valves. While these are the most common causes of ischemic stroke, there are many other possible causes. Examples include use of street drugs, traumatic injury to the blood vessels of the neck, or disorders of blood clotting.