Hypoxic-ischemic Injury in Neonates
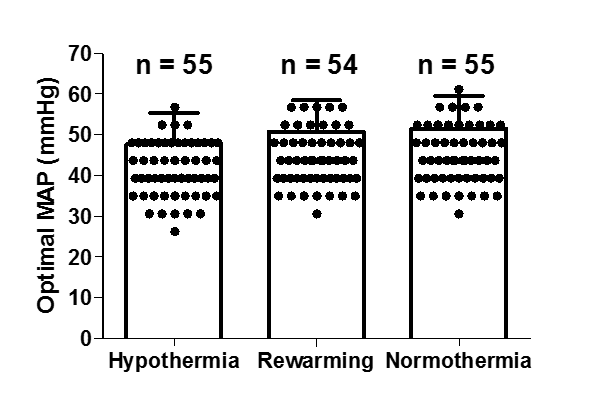
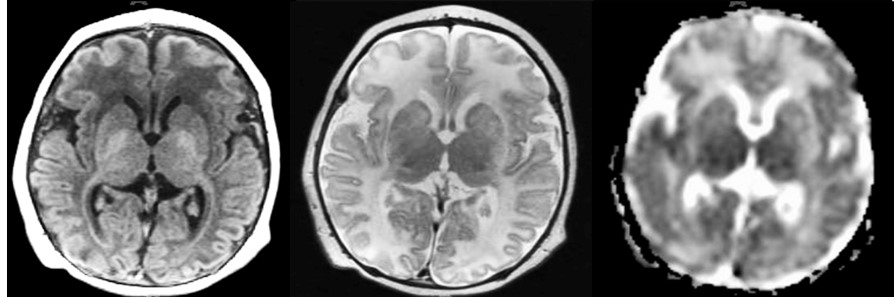
We study cerebrovascular blood pressure autoregulation in neonates who receive therapeutic hypothermia for hypoxic-ischemic encephalopathy (HIE). The babies receive cerebral NIRS and arterial blood pressure monitoring to calculate the hemoglobin volume autoregulation index (HVx). We try to identify each baby’s ‘optimal’ mean arterial blood pressure as the mean arterial pressure (MAP) with the best autoregulation – in other words the lowest HVx – (MAPOPT) during hypothermia, rewarming, and the first 6 hours of normothermia (figure 1). In our prospective study the absolute MAPOPT values and the deviation in MAP from MAPOPT are correlated to MRI evidence of (hypoxic) brain injury at 1–2 weeks (figure 2) and neurodevelopmental outcome at ~2 years. [1-6]
Identifying Optimal Mean Arterial Blood Pressure (MAPOPT): Neonates with Hypoxic-Ischemic Encephalopathy (HIE). [7-10]
Important findings
Maintaining MAP within the MAPOPT range may decrease the risk of injury in white matter, putamen and globus pallidus in neonates. Deviation from MAPOPT is associated with greater injury in paracentral gyri and white matter (n=64).
The effects of deviation from MAPOPT on cardiopulmonary injury may be sex specific in neonates.
Maintaining MAP close to MAPOPT may support renal recovery in neonates.
For more information about these studies:
Please contact Dr. Jennifer K. Lee, MD, Johns Hopkins University, USA.
✉ jklee@jhmi.edu
References
[1] Howlett JA, Northington FJ, Gilmore MM, et al. Cerebrovascular autoregulation and neurologic injury in neonatal hypoxic-ischemic encephalopathy. Pediatr Res 2013; 74: 525-535.
[2] Tekes A, Poretti A, Scheurkogel MM, et al. Apparent Diffusion Coefficient Scalars Correlate with Near Infrared Spectroscopy Markers of Cerebrovascular Autoregulation in Neonates Cooled for Perinatal Hypoxic Ischemic Injury. Am J Neuroradiol 2015; 36(1):188-93.
[3] Burton VJ, Gerner G, Cristofalo E, et al. A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia. BMC Neurology 2015; 15:209–22.
[4] Lee JK, Poretti A, Perin J, Huisman TAGM, et al. Optimizing cerebral autoregulation may decrease neonatal regional hypoxic-ischemic brain injury. Dev Neurosci 2016; DOI: 10.1159/000452833 .
[5] Chavez-Valdez R, O’Connor M, Perin J, et al. Associations between cerebrovascular blood pressure autoregulation and cardiopulmonary injury may be sex-specific in neonates treated with therapeutic hypothermia for hypoxic-ischemic encephalopathy. Pediatr Res 2017; 81(5):759-766.
[6] Lee JK, Perin J, Parkinson C, et al. Relationships between cerebral autoregulation and markers of kidney and liver injury in neonatal encephalopathy and therapeutic hypothermia. J Perinatol 2017; in press. DOI: 10.1038/jp.2017.64 .
[7] Lee JK, Poretti A, Perin J, et al. Optimizing cerebral autoregulation may decrease neonatal regional hypoxic-ischemic brain injury. Dev Neurosci. 2016.
[8] Howlett, FJ Northington, MM Gilmore, et al. Cerebrovascular autoregulation and neurologic injury in neonatal hypoxic-ischemic encephalopathy. Pediatr Res. 2013.
[9] Chavez-Valdez R, O’Connor M, Perin J, Reyes M, et al. Sex-specific associations between cerebrovascular blood pressure autoregulation and cardiopulmonary injury in neonatal encephalopathy and therapeutic hypothermia. Pediatr Res. 2017.
[10] Lee JK, Perin J, Parkinson J, et al. Relationships between cerebral autoregulation and markers of kidney and liver injury in neonatal encephalopathy and therapeutic hypothermia. J Perinatol. 2017.
